Last reviewed by a Registered Dietitian on 30 June 2025
Why This Guide?
If you live with Irritable Bowel Syndrome (IBS), you already know how unpredictable life can feel. Abdominal pain, bloating, and urgent bathroom trips derail workdays and weekends alike. Research shows that up to 75 percent of people with IBS achieve noticeable relief within two to six weeks on a Low FODMAP diet—yet most beginners quit early because the learning curve appears steep.
This Low FODMAP Quick‑Start Guide breaks the entire process into three clear phases you can start today. You’ll find concise explanations, practical examples, and links to deeper dives on Calm Belly Cooking, so you never feel lost.
Estimated reading time: 5 minutes.
Disclaimer: The Low‑FODMAP diet is a short‑term learning tool, not a lifelong prescription. Always consult a registered dietitian or your physician before making major dietary changes, especially if you have other medical conditions.
Table of Contents
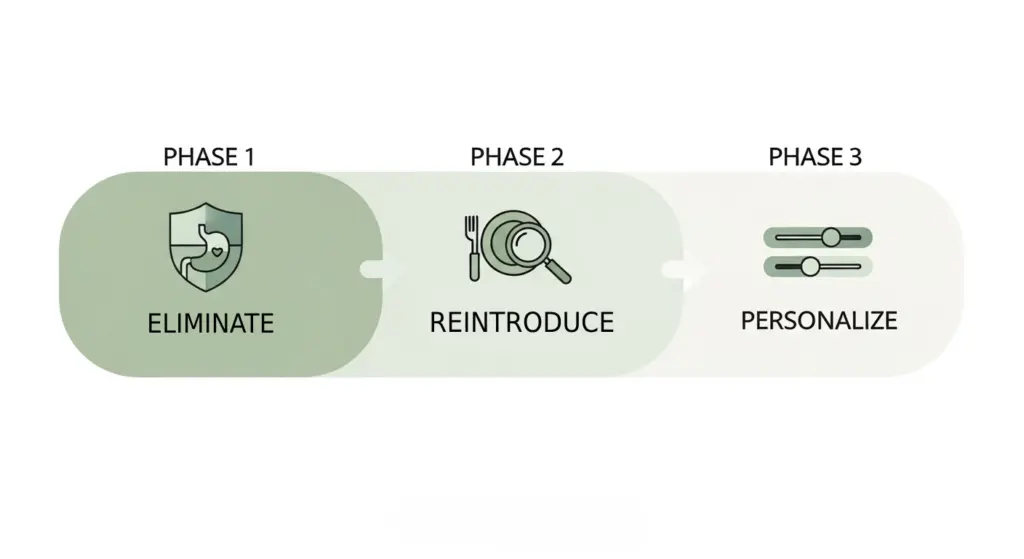
Phase 1 – Eliminate High‑FODMAP Triggers (Weeks 0 – 2 to 6)
A calm digestive tract is your foundation. By temporarily removing most high‑FODMAP foods, you reduce fermentation in the gut and give inflamed nerves a chance to settle. Most people notice less gas and cramping within the first 7 to 14 days.
1.1 Reset Your Kitchen
Before day 1, take one evening to audit the pantry and fridge. Keep a printed copy of our Low FODMAP Food List on the counter for quick reference. High‑FODMAP ingredients—like regular wheat bread, apples, and garlic—go to a “pause box” you’ll revisit later. Restock with lactose‑free milk, gluten‑free bread, maple syrup, and garlic‑infused oil so meals don’t feel restrictive.
1.2 Build Five Reliable Core Meals
Repetition may sound boring, yet it’s the fastest route to pattern recognition. Aim for two breakfasts, two lunches, and one dinner that hit all major macros and use low‑FODMAP ingredients. Example: Overnight oats made with lactose‑free milk, chia seeds, and strawberries (½ cup) keep mornings stress‑free.
1.3 Track What You Eat & How You Feel
Print our free food & symptom tracker (PDF) or use a phone app. Write down:
- Exact foods & portion sizes
- Meal times
- Symptoms (0–10 scale)
- Stress level & sleep quality (bonus insight)
TIP: Numbers reveal trends faster than adjectives. “Bloating 8/10 → 3/10” after three days is both motivating and informative.
1.4 Timing
Stay in Phase 1 until you achieve at least 50 percent symptom improvement or you reach week 6—whichever occurs first. Longer restriction does not equal better results and may harm gut‑microbiome diversity.
Phase 2 – Reintroduce & Challenge Methodically (Weeks 3 – 8)
Phase 2 transforms a generic Low FODMAP diet into a personal blueprint. You’ll test one FODMAP group at a time—lactose, excess fructose, fructans, galacto‑oligosaccharides (GOS), and polyols.
2.1 Standard 4‑Day Challenge Template
| Day | Action | Example Portion |
|---|---|---|
| 1 | Introduce test food | ½ cup lactose‑containing milk |
| 2 | Increase dose | 1 cup milk |
| 3 | “Stress test” | 1½ cups milk |
| 4 | Return to baseline diet | Observe 48 hours |
Record symptoms immediately, 2 hours later, and the next morning.
2.2 Make Challenges Bulletproof
- Isolate one variable. Testing garlic bread confuses wheat fructans with garlic fructans.
- Pause if life gets messy. Illness, antibiotics, or high stress can mimic FODMAP reactions.
- Document honestly. Minor bloating may be acceptable; severe cramps probably aren’t.
2.3 Color‑Code Your Results
| Outcome | Color | Meaning |
| No change | Green | Safe food in tested portion |
| Mild symptoms | Yellow | Enjoy in small amounts |
| Moderate–severe symptoms | Red | Avoid for now |
Transfer colors to a master spreadsheet you’ll use in Phase 3.
Phase 3 – Personalize & Maintain (Ongoing)
Armed with your color chart, you can relax dietary rules without sacrificing symptom control.
3.1 Craft Your Personal Low FODMAP Playbook
- Green foods become daily staples.
- Yellow foods rotate in during social occasions or travel.
- Red foods stay off the menu—but test again every 6‑12 months; tolerances change.
3.2 Real‑World Survival Tips
Dining out: Search menus ahead of time; grilled proteins and rice bowls are usually safe. Politely request “no onion or garlic.”
Travel: Pack low‑FODMAP snacks and learn local words for wheat, milk, onion, and garlic.
Label reading: Watch for hidden culprits such as inulin, chicory root, sorbitol, and xylitol.
(Insert an infographic here—alt=”Low FODMAP diet infographic showing the three‑phase process: elimination, reintroduction, personalization”.)
3‑Day Low FODMAP Meal Plan (Balanced ≈ 1 650 kcal/day)
Kick‑start your week with this 3‑day Low FODMAP meal plan—carefully balanced at roughly 1,650 kcal per day to suit the average adult while keeping every serving inside Monash‑approved limits. Each menu blends lean protein, low‑FODMAP carbs, healthy fats, and plenty of micronutrient‑rich produce so you stay satisfied, energized, and on track for IBS relief. Feel free to mix and match ingredients from our Low FODMAP Food List, keeping the same portion sizes, to add variety without upping FODMAP load.
| Day | Breakfast | Lunch | Snack | Dinner |
| 1 | Overnight oats, lactose‑free milk, chia, strawberries | Quinoa‑chicken salad with cucumber & feta (40 g) | Rice cakes + peanut butter | Lemon‑herb salmon, roasted carrots, mashed potatoes |
| 2 | Scrambled eggs, sautéed spinach, gluten‑free toast | Shrimp rice‑noodle stir‑fry with bok choy | Blueberries + lactose‑free yogurt | Turkey burger (no bun) with cheddar (40 g) & mixed greens |
| 3 | Green smoothie: pineapple, baby kale, almond milk | Beef tacos in corn tortillas, lettuce, salsa verde | Walnuts + kiwi (1) | Baked cod, zucchini ribbons, creamy polenta |
All portions align with Monash University low‑FODMAP serving sizes.
Need more inspiration? Browse our ever‑growing Low FODMAP recipe archive.
Frequently Asked Questions
What foods are Low FODMAP?
Low FODMAP foods include plain meat, fish, eggs, most leafy greens, rice, quinoa, oats, berries, citrus, hard cheeses, lactose‑free dairy, and small portions of nuts and seeds. See our complete Low FODMAP Food List for serving sizes.
What can I eat out on a Low FODMAP diet?
Choose grilled protein, steamed rice or potatoes, plain veggies, and simple sauces (no onion or garlic). Ask for dressings on the side and request gluten‑free bread if wheat triggers you. Sushi, bun‑less burgers, and steak‑house menus often have Low FODMAP options.
What causes FODMAP symptoms?
FODMAP symptoms arise when poorly absorbed carbohydrates pull water into the gut and ferment in the colon, creating gas. The resulting distension stimulates pain‑sensitive nerves in people with IBS, leading to bloating, cramps, and altered bowel habits.
How can I tell if I’m FODMAP‑sensitive?
Track symptoms during a two‑ to six‑week Low FODMAP elimination phase. If abdominal pain, bloating, or bowel changes improve by 50 percent or more, you likely react to one or more FODMAP groups. Re‑challenge foods to pinpoint specific triggers.
Is the Low FODMAP diet safe during pregnancy?
Generally yes, but work with a registered dietitian to meet fiber, calcium, and folate needs. Monitor weight gain and diversify foods during the personalization phase.
How soon will I feel better on a Low FODMAP diet?
Most people notice less gas and bloating within seven to fourteen days of strict elimination, with continued improvement through week four.
Next Steps & Resources
- Explore: Our Low FODMAP Food List for portion specifics
- App: Monash University FODMAP (iOS / Android) for on‑the‑go look‑ups
- Join: Subscribe to our newsletter for weekly gut‑friendly recipes and tips
Share Your Wins!
Tag @CalmBellyCooking and use #CalmBellyRelief on social media so we can celebrate with you.
Article by Calm Belly Cooking Team
Medically reviewed 30 June 2025 by a Registered Dietitian, RD, CNSC
References
- Chey WD et al. Am J Gastroenterol. 2025;120(1):34‑45.